Mental health: An invisible epidemic
Mental health has long been a subject no one likes to talk about. It exists, but remains wrapped in silence. According to data from the National Mental Health Survey (NMHS), about 10.6 per cent of adults in India — translating to over 150 million people — are currently living with one or more mental health disorders requiring intervention. This is not just serious but alarming, as it affects the social and economic fabric of the country. It often leads to serious crimes and a drop in efficiency at the workplace, not to mention the trauma endured by family members and loved ones. Unfortunately, mental illness is rarely treated adequately due to the stigma attached to it.
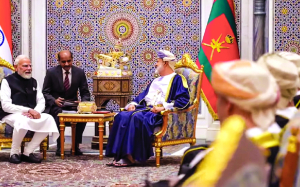
In a long-overdue step, the Indian government has relaunched the National Mental Health Survey after a nine-year hiatus, extending its reach to all states and Union Territories for the first time. The survey — NMHS-2 — aims to map the prevalence, impact, and service utilisation patterns of mental health conditions across the country, including among vulnerable groups such as children, women, migrants, and the elderly. This is likely to be helpful in framing and fine-tuning the National Mental Health Programme, as well as guiding resource allocation and policy decisions. This initiative, though welcome, arrives late, at a moment when mental health concerns in India have sharply escalated. Post-pandemic stress, economic uncertainty, and rapidly changing social norms have together intensified psychological vulnerability and significantly increased the risk of mental illness across sections of society.
Yet data alone will not resolve the crisis. On the ground, the scale of need is already visible through one of the most tangible government interventions: Tele-MANAS, the National Tele Mental Health Programme. Launched on October 10, 2022, this toll-free helpline and digital support platform has emerged as a critical lifeline for millions. According to recent official figures, Tele-MANAS logged over 24 lakh calls between late 2022 and mid-2025, averaging more than 2,500 calls daily from across 37 states and territories.
The callers — from working adults in distress to young people grappling with academic and job-related pressures — starkly illustrates the pervasive mental health burden India faces. These figures are significant not just for their scale, but for what they reveal about trust and access. Many callers come from remote or underserved regions where mental health services are limited or entirely absent.
However, helplines are no substitute for a comprehensive system of care that includes community-based services, trained professionals, outreach, and preventive interventions.
India still lacks a uniformly implemented mental health policy with clear benchmarks, robust funding, and an adequate caregiving workforce. Schools and universities need trained counsellors. Insurance coverage for mental health must be strengthened, and public awareness campaigns must move beyond slogans to sustained behavioural change. India can no longer afford to treat mental health as a secondary concern.