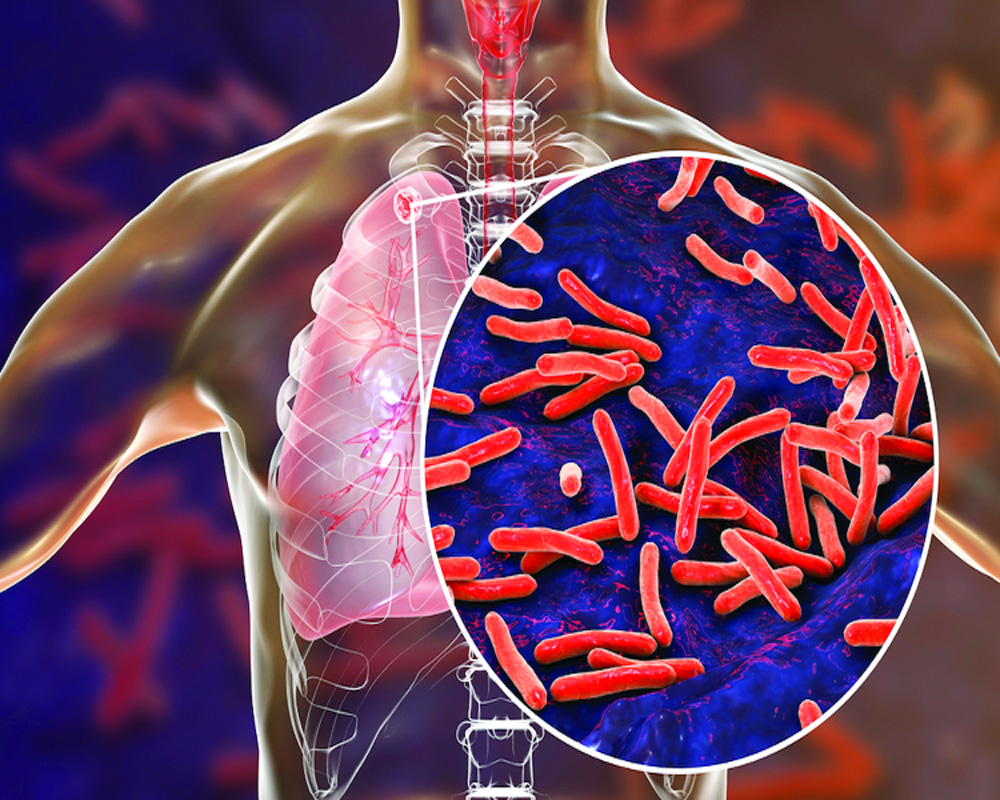
The disease heavily affects the most marginalised groups due to lack of awareness and stigma attached to it
Despite the availability of many schemes, Tuberculosis (TB) is still one of India’s most pressing public health crises, with the highest incidence of 2.8 million cases annually, accounting for more than a quarter of the global TB burden. According to the India TB report 2020, around 3 lakh TB cases in India, were either undetected and untreated. TB heavily affects the most marginalised groups due to lack of awareness and stigma attached to the disease. People with TB face many side-effects like nausea, loss of appetite and fatigue. Due to this, they need to have access to a nutritious diet, as undernutrition weakens the body’s ability to fight the disease. Hence, it is important to increase people’s access to nutrition, and basic facilities like transportation for successful treatment.
To ensure this, the Government of India provides targeted benefits to people through the Direct Benefit Transfer (DBT). The government subsidy or benefit is transferred directly into the bank account of the beneficiary. There are four DBT schemes currently, namely- Nikshay Poshan Yojana (NPY), Incentives for private sector providers and informants, treatment supporters honorarium and transport support for TB patients in notified Tribal areas. The objective of the NPY is to provide nutritional support to TB patients during the course of their treatment. An amount of Rs. 500 is paid for each month of treatment.
There are organisations like Karnataka Health Promotion Trust (KHPT) that are committed and working to increase people’s access to these schemes under ongoing projects like Breaking the Barriers (BTB). There are multiple case stories of patients, like Mahesh (name changed) who needed access to nutritious food because of the side-effects faced due to the treatment process, and have found it difficult to access the DBT payment. KHPT’s intervention has assisted patients from vulnerable populations to link their bank accounts for access to these payments under the NPY. In Mahesh’s case the team approached the National Tuberculosis Elimination Program (NTEP) team to ensure that Mahesh’s bank account was linked to the NPY. Additionally, a free supply of the Fixed Dose Combination (FDC) was provided to him, which helped him reduce his out-of-pocket expenses. Today, Mahesh is happy to receive the support, which he uses to buy food, and is on his way to recovery.
TB diagnosis can lead to social stigma which can worsen people’s psycho-social health and make them more vulnerable to suffering from the disease. In the absence of support from the community and people around them, the physical, mental and emotional toll faced by them rises significantly.
Another example is Rajan (name changed) whose only source of livelihood is agriculture. After being detected with TB, he faced financial constraints. In addition, nobody around him, his neighbours, or his son provided any support. The BTB team sensitised the neighbours on the need to support the couple, negating fear and myths about the disease. They were also encouraged to provide basic necessities to Rajan and his family, as the regular intake of medication, without a proper diet, was making him weaker. The team further informed the official in-charge of the Tuberculosis Unit of Rajan’s situation, ensuring smooth collection of the details required for DBT towards NPY. Due to the support provided through linkage to schemes and sensitization of people surrounding him, he has been able to access nutrition and is undergoing treatment at the moment.
The availability of any scheme does not necessarily translate into people accessing it, many times due to constraints like lack of awareness, perceived fear of lengthy process, and stigma. Hence, it is crucial to adopt holistic implementation of strategies to ensure that these schemes reach the grassroots level and are accessible to all.