According to the Indian Council of Medical Research survey, about 20% children with Sickle Cell Disease died before attaining the age of two. DR SHEETAL SHARDA tells you what one can do to prevent the complications of this disorder
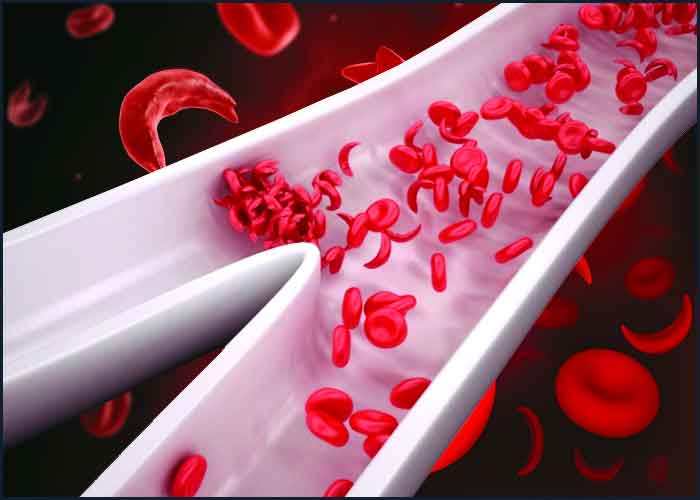
Sickle cell anaemia (SCA) or sickle cell disease (SCD) is an inherited blood disorder in which the red blood cells take an abnormal sickle shape instead of the normal spherical form. The hemoglobin in our body consists of four proteins sub-units, typically, two subunits called alpha globin and two subunits called beta-globin encoded by the HBA and the HBB gene respectively.A mutation or change in the HBB gene leads to blood disorders like beta-thalassemia and sickle cell. A specific mutation in the HBB gene encodes for an abnormal hemoglobin which causes the RBCs to take an abnormal shape.
In a normal person, the red blood cells (RBCs) have a lifespan of about 90-120 days. However, in a SCA patient, the RBCs do not last long and break down, due to the abnormal sickle shape. This lack of RBCs in the blood leads to anaemia, which may manifest as swelling of the hands and feet and fatigue. In a SCA patient, the sickle shaped RBCs may block the small blood vessels, which over time leads to complications like delayed growth, frequent pain crisis and can cause multiple organ damage. Patients may require blood transfusions to overcome the acute crisis and to keep the hemoglobin in normal range.
Sickle cell anemia is very common among people of African, Arabian and Indian origin.The first evidence of SCA in India was seen in the tribal population in the Nilgiri Hills in South India. Based on certain surveys, prevalence of sickle gene is found to be 0-18 per cent in north eastern India, 0-33.5 per cent in western India, 22.5-44.4 per cent in central India and 1-40 per cent in southern India. Wide variability in the prevalence of Hb-S trait is observed in population groups within small geographical areas
Sickle cell disease is inherited in an autosomal recessive pattern, which means that both copies of the HBB gene have tobe mutated in order for the disease to manifest. Carriers or persons with a single mutated copy may be asymptomatic and are called sickle cell traits. If both parents carry a copy of the mutated gene, then their child will have a 25 per cent chance of being affected with SCD.
To prevent the complications of sickle cell anaemia,early diagnosis of the disease is very necessary. Patients who test positive for abnormal haemoglobin by biochemical testing, need to undergo genetic testing to confirm their diagnosis. Screening for SCA can also be done in new-born period with a simple blood test that detects the presence of the abnormal haemoglobin. Being picked up during an asymptomatic period, such children can have timely and early intervention in case of a crisis and thus prevent secondary complications
Carrier screening is a good way to assess if an individual is a carrier of the disease. Usually it is undertaken on individuals who have a family history of SCD or thalassemia and in certain ethnic groups with an increased risk of SCA. But in some cases there may be no family history and carrier status is confirmed only after the birth of an affected child, which is then too late to prevent the disease and its complications. Hence, carrier screening for SCA and thalassemia should be offered to every couple who are planning pregnancy,in order to prevent the birth of an affected child or even to take decision of giving birth to an affected child but being prepared for the future management required.Screening of such couples at the right time (pre-conceptional carrier screening) can help them take informed decision regarding their future children. Some couples also opt for pre-marital genetic counselling and genetic testing when they are aware of such genetic conditions in their family.
Let’s make it a point to create awareness on the need for effective and early diagnosis of SCD, so that appropriate management can be offered to patients and families suffering from SCD.
Prevention of genetic diseases causing high morbidity and mortality is possible based on genetic testing and availability of prenatal diagnosis. This can help decrease the incidence of genetic disorders in India and help us to reduce the psychological and financial burden on the families.
The writer is Consultant Clinical Geneticist, MedGenome Labs, Bengaluru