WHO declares the outbreak of monkeypox as a public health emergency of global proportions, underscoring need for preparedness
India is enhancing its preparedness to tackle Monkeypox (Mpox) by raising awareness, strengthening surveillance, setting up isolated wards, and expanding diagnostic testing capacity. Although a pandemic-like situation has not emerged, all mechanisms are being put in place to curtail the spread of Mpox and its menace. Since January 2023, the Democratic Republic of the Congo (DRC) has reported more than 27,000
suspect Mpox cases and more than 1,300 deaths. Clade I Mpox occurs regularly, or is endemic, in DRC.
The current outbreak is more widespread than any previous DRC outbreak, and Clade I Mpox has spread to some neighbouring countries, including Burundi, the Central
African Republic, the Republic of the Congo, Rwanda, and Uganda, and a travel-associated case in Kenya. On August 14, 2024, the World Health Organization (WHO) declared the outbreak a Public Health Emergency of International Concern (PHEIC). This is the WHO’s highest level of global alert, and the decision recognizes the potential threat this virus poses to countries around the world.
The declaration focuses international attention on acute public health risks that require the coordinated mobilization of extraordinary resources by the international community for prevention and response. Monkeypox is a virus that transmits from animals to humans. Technically, it is known as a ‘viral zoonosis’. Its symptoms are similar to smallpox and cowpox, but fortunately, Monkeypox is less severe.
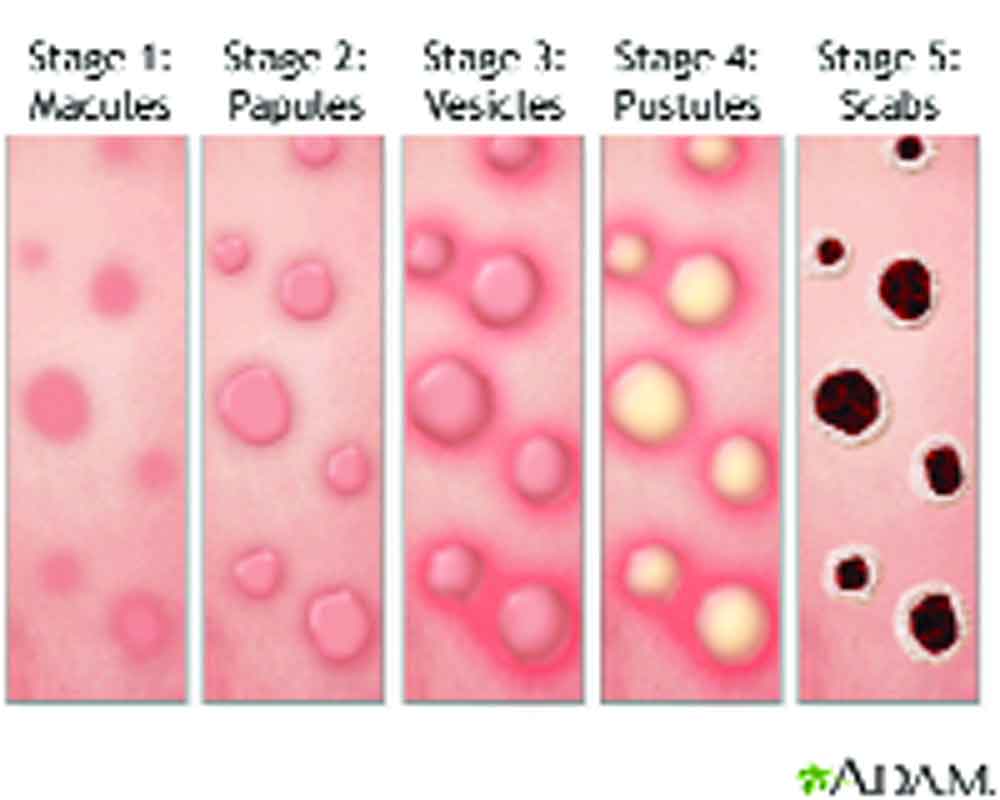
Cases have been emanated from Central Africa and are reported to be spreading fast across the globe. Common symptoms of Mpox are a skin rash or mucosal lesions which can last 2–4 weeks accompanied by fever, headache, muscle aches, back pain, low energy, and swollen lymph nodes. So far, no cases have been reported from India.
The Monkeypox virus was discovered in Denmark (1958) among monkeys kept for research. The first reported human case of Mpox was in a nine-month-old boy in the DRC in 1970. Following the eradication of smallpox in 1980, Mpox steadily emerged in central, east and west Africa. In 2003, an outbreak in the United States of America was linked to imported wild animals (Clade II). Since 2005, thousands of suspected cases have been reported in the DRC every year.
In 2017, Mpox re-emerged in Nigeria and continues to spread among people across the country and travellers to other destinations. The natural reservoir of the virus is unknown – various small mammals such as squirrels and monkeys are susceptible. In May 2022, an outbreak of Mpox appeared suddenly and rapidly spread across Europe, the Americas and then all six WHO regions, with 110 countries reporting about 87 thousand cases and 112 deaths.
The global outbreak has affected primarily gay, bisexual, and other men who have sex with men and has spread person-to-person through sexual networks. The global Clade II Monkeypox virus (MPXV) outbreak that began in 2022 demonstrated the pandemic potential of Mpox. Clade I MPXV is endemic in several Central African countries, including the Democratic Republic of the Congo (DRC). Clade I is generally associated with higher case fatality rates (CFRs) (1.4% to >10%) compared with Clade II MPXV (0.1% to 3.6%).
MPXV can spread to persons from contact with infected wildlife, or through close, prolonged contact with persons infected with MPXV. During 2023–2024, DRC has reported an unprecedented number of suspected Clade I MPXV infections. Clade I MPXV transmission in DRC is more commonly reported among children. Widespread transmission is reported because of zoonotic reservoirs, household occupants, and unhygienic resources.
Diagnosis and reporting of Clade I MPXV infections to health officials are important for limiting onward transmission by aiding early containment measures, including contact tracing, isolating patients, offering the JYNNEOS vaccine to contacts, and strictly adhering to recommended infection prevention and control practices in health care settings.
An additional benefit of vaccination is protection against Clade I MPXV infection. According to Dr A K Narula, Pharmacy expert of GGSIPU, Tecovirimat is typically the first therapeutic that should be considered for patients with Mpox other than supportive care.
In 2014, the West Africa Ebolavirus outbreak demonstrated the risks associated with a delayed global response to a serious pandemic threat. Identifying Mpox is a difficult task, as other infections and conditions look similar.
It is important to distinguish Mpox from chickenpox, measles, bacterial skin infections, scabies, herpes, syphilis, other sexually transmissible infections, and medication-associated allergies. For these reasons, testing is key for people to get treatment as early as possible and prevent further spread.
(The writer is former editor Free Press Journal and presently media advisor to GGSIPU; views are personal)